Table of Contents
- Eclampsia Definition
- Epidemiology of Eclampsia
- Eclampsia Causes and Risk factors
- Risk factors of Eclampsia
- Eclampsia Pathophysiology
- Types of Eclampsia
- Eclampsia Symptoms
- Signs of Eclampsia
- Laboratory Tests for Eclampsia
- Eclampsia Management
- Eclampsia Treatment Guidelines
- Eclampsia Complications
- Differential diagnosis of Eclampsia
Eclampsia Definition
Eclampsia is the occurrence of Convulsion with Preeclampsia or Pregnancy-induced hypertension. When a woman with signs and symptoms of preeclampsia or pregnancy induced hypertension experiences convulsive attacks or fits in addition, she is said to suffer from Eclampsia.
The nature of the convulsion or fit in Eclampsia follows these patterns:
- Twitching: 30 seconds.
- Tonic phase: 30 seconds.
- Clonic phase: 2 minutes.
- Coma: 10 to 30 minutes
Epidemiology of Eclampsia
The incidence of Eclampsia varies widely across the world with high incidence in developing countries and low incidence in developed countries largely because of excellent antenatal care in developed countries. The incidence of Eclampsia in the United Kingdom is about 1 in 2000 pregnancies while that of referral institution in Nigeria is about 11.8 per 1000 deliveries with higher values in hospitals or clinics in rural areas.
Eclampsia Causes and Risk factors
The etiology of Eclampsia is unknown since that of preeclampsia is unknown (Preeclampsia has been known as The Disease of Theories as the exact course of events that lead to the clinical syndrome have not been elucidated). However there are risk factors of Eclampsia as outline below.
Risk factors of Eclampsia
- First pregnancy
- Nulliparity
- Young age or Age 40 or older
- Family history of pre-eclampsia such as a mother or sister who has had Eclampsia or preeclampsia)
- A prior history of pre-eclampsia
- Body mass index (BMI) above 35
- Multiple pregnancy
- Pre-existing vascular disease such as hypertension or Diabetes
Eclampsia Pathophysiology
The pathological features found in Eclampsia occur as a result of spasm of the vascular supply to organs; organs such as the kidneys show marked spasm of glomerular arterioles leading to the narrowing of the lumina. The glomeruli are enlarged and cellular and the capillary of the end-arterial cells are swollen; there could also be Tubular necrosis or more widespread acute cortical necrosis.
The liver shows sub-capsular hemorrhages and hemorrhagic infarcts throughout its substance and there could be peri-portal hemorrhages and necrosis. There are vascular changes in the brain that cause marked edematous. Hemorrhages which may be tiny or large are very often present and many patients succumb to this complication.
The lungs show evidence of congestion, infection or aspiration pneumonia. Hemorrhagic areas are often found in the heart and adrenal glands.
Types of Eclampsia
- Antepartum Eclampsia: this type of Eclampsia occurs before labour
- Intrapartum Eclampsia: this occurs during labour
- Postpartum Eclampsia: this type of Eclampsia occurs after delivery
The commonest type of Eclampsia in Nigeria is the Intrapartum type followed by the Antepartum type and then the Postpartum Eclampsia depending on the locality.
Eclampsia Symptoms
- Severe headache
- Epigastric pain (Chest pain)
- Vomiting
- Blurring of vision
- Convulsion or fits
- There could be unconsciousness or coma
Sometimes these Eclampsia symptoms appear very suddenly especially in a woman without previous antenatal care
Signs of Eclampsia
- Hypertension
- Edema of the legs, hands and face
- Significant proteinuria
Laboratory Tests for Eclampsia
- Urinalysis: this shows significant proteinuria.
- Blood tests for hemoglobin or packed cell volume (PCV), White cell count, platelet count, urea, uric acid, creatinine and electrolyte estimation.
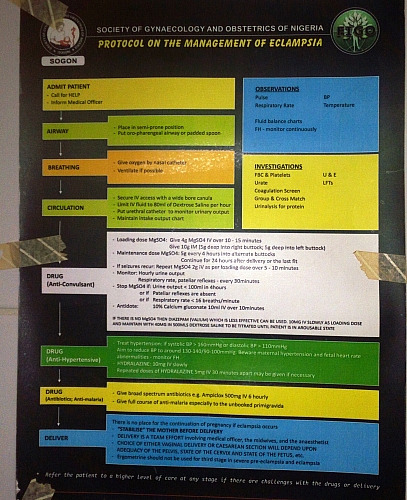
Eclampsia Management
The Principle of Eclampsia management is aimed at achieving the following:
- Control of convulsions
- Control of hypertension
- Fluid and electrolyte balance
- Delivery of the fetus
Eclampsia Treatment Guidelines
Control of Convulsions in Eclampsia
Stopping further convulsions in a woman with Eclampsia is very important as the greater the number of convulsions, the worse the prognosis of Eclampsia. The drug of choice for the control of convulsions in Eclampsia is Magnesium Sulphate (MgSO4). Other drugs used when Magnesium sulfate is not available include Diazepam and Phenytoin.
The Pritchard regimen is usually used. There are other regimens used in the control of convulsions in Eclampsia such as the Sokoto regimen. What will be described here is the Prichard regimen.
The Pritchard regimen
- 4g of magnesium sulphate is double diluted and given intravenously over 5-10 minutes as loading dose; 10g is then given intramuscularly (5g in each buttock).
- A maintenance dose of 5g is given every 4 hours in alternate buttocks and continued until 24 hours after delivery or 24 hours after the last fit (or convulsion).
Any patient receiving magnesium sulphate should be closely monitored for magnesium sulphate toxicity . Respiratory rate, knee jerks and urine output are used in monitoring. Any sign of toxicity calls for stoppage of MgSO4 and the antidote should be given (10mls of 10% Calcium gluconate or 10mls of 10% Calcium chloride is given intravenously). The respiratory rate should be above 12 cycles per minute, urinary output should be at least 25mls per hour or 100mls/4hrs while knee reflexes should be present.
Control of Hypertension
The drug of choice in the control of hypertension in Eclampsia is Hydralazine. If the diastolic blood pressure is greater than 100mmHg, Hydralazine will be given as 5mg intravenous bolus. The blood pressure is repeated after 30min and if there is no fall it is followed by an intravenous infusion of 40mg hydralazine in 500ml normal saline commencing at 10 drops per minute and increased gradually until a fall is achieved. The diastolic blood pressure should preferably be brought down to between 80 and 90 mmHg. Any attempt to control the blood pressure more dramatically may result in fetal compromise.
Fluid and Electrolyte balance
Hypovolemia is a characteristic feature of Eclampsia, therefore there is need for fluid balance; this is achieved by replacing the equivalent loss through urine and vomiting in the last 24hours plus an additional 1,500ml which represents the amount of insensible loss from skin and lungs in the tropics. The fluids usually used include 5% dextrose water (alternated with 5% dextrose in lactated ringers solution). An indwelling urethral catheter is mandatory for accurate measurement of urinary output.
Delivery of the Fetus
Once there is control of convulsion and the woman is stabilized, the next form of treatment is delivery of the fetus. If the cervix is favorable and there are no contraindications to vaginal delivery, the membranes are then ruptured artificially and labour is then augmented with oxytocic infusion. The fetus should be carefully monitored in labour with cardiotocograph and the second stage of labour should be shortened by forceps or ventouse. If after 8-10 hours there is no delivery following induction or if labour is not progressing satisfactorily, a caesarean section should preferably be instituted. Once there is Eclampsia, the only permanent form of treatment is delivery of the baby whatever the gestational age may be in order to prevent harm to the mother as well as the fetus.
Eclampsia Complications
- Abruption placentae
- Intra-Uterine Growth Restriction (IUGR)
- Intra-Uterine Fetal Death (IUFD)
- Left Ventricular Failure
- Renal failure may be due to tubular necrosis or massive cortical necrosis
- Disseminated Intravascular Coagulopathy (DIC)
- HELLP syndrome (Hemolysis, Elevated liver enzymes, Low Platelets)
- Preterm labour
Differential diagnosis of Eclampsia
- Idiopathic epilepsy
- Meningitis
- Encephalitis
- HIV encephalopathy
- Cerebral malaria
- Diabetic coma
- Hypoglycemic coma